Summary
EFFECTIVE DATE: June 1, 2023
Under Section 204 (of Title II, Division BB) of the Consolidated Appropriations Act 2021 (CAA), insurance companies and employer-based health plans offering group or individual health coverage and self-funded or Administrative Services Only (ASO) group health plans are required to report information about prescription drugs and health care spending to the Departments of Health and Human Services, Labor, and Treasury (Tri-Agencies). This data submission is called the RxDC report. The Rx stands for prescription drug and the DC stands for data collection. This report is due to CMS by June 1, 2023 for the 2022 reference year. CMS has allowed the insurance carriers to file these reports on behalf of employers. However, some of the data, required in the report, is data that the insurance companies do not have. The carriers are in the process of sending out “surveys” to our clients asking them to complete and send them back to the carriers. With the completed data the insurers submit all of the requested data to CMS by the June 1st due date.
Overview
Under the Consolidated Appropriations Act 2021 (CAA), health issuers offering group or individual health coverage and self-funded group health plans must submit detailed data on prescription drug pricing and healthcare spending.
This report titled, The RxDC report is due June 1st each year. The reporting requirements include information intended to identify the significant drivers of increases in prescription drug and healthcare costs, increase understanding of how prescription drug rebates impact premiums and out-of-pocket costs, and improve prescription drug pricing transparency.
In the original version of this legislation employers were required to report this data to CMS. In the most recent FAQs, the agency simplified the requirements for employers by allowing most of this data to be reported in aggregate by the individual plan or insurer. This was designed to alleviate some of the challenges an employer might face in gathering this data.
Period to be Reported
The reporting periods are calendar years and are referred to as “reference years”. The first report due data for reference years 2020 and 2021 was due by the carriers on January 21, 2023. The 2022 2022 reference year data is due on June 1, 2023 and on June 1st each of each subsequent year. Required entities must submit the report through a web portal managed by the Centers for Medicare & Medicaid Services (CMS), which will collect the data on behalf of the Departments of Health and Human Services, the Department of Labor, and the Department of the Treasury (the “Departments”).
Who Must Report
Insurers are in the process of gathering data from employers for the upcoming June 1, 2023 report filing deadline for reference year 2022. Some of the data that CMS is asking for is not data that the insurers have and, in order to complete the report are asking employers to assist with this process by completing electronic “surveys”. Insurers are in the process of sending out notifications to employers asking them to complete the survey by a specific deadline. This disclosure requirement covers all insured groups with coverage at any time in 2022 including fully insured, level funded and ASO groups.
How is the Reporting Done?
How is the Reporting Done?
Plans, issuers, and carriers must submit one or more plan lists, eight data files, and a narrative response. Data is reported through the RxDC module in the Health Insurance Oversight System (“HIOS”). An account must be created unless the employer meets the following criteria: already has an HIOS account or, is not reporting because a vendor is handling the filing, or the employer is uploading partial data, not including any files.
For all Parrott Benefit Group clients who are either fully or partially (level or balanced funded) insured, the insurance carrier (i.e., BCBSNC, Aetna, Cigna, UHC) will be handling the filing on your behalf after you have returned the completed survey(s) to the carrier(s).
What You Need to Know
Insurer Survey Questions
Each insurer has created their own unique survey for employers to complete. Each company will have their own look to the survey the questions asked within the survey will be similar if not the same. Much of the data being asked for in the survey is easily accessible and widely known (by the employer) data such as EIN and whether the policy in place is either fully insured, self-insured or level funded. There are however two questions that employers will need to be prepared to answer that include a calculation they must use. The two questions are:
- Average monthly premium paid by members
- Average monthly premium paid by employer
CMS has provided specific criteria and a formula for calculating these two numbers. In order for this number to be accurately reported employers will need to use this calculation.
Average Monthly Premium Paid by Members
For the purposes of this report, the term “member” means a person who has health coverage, regardless of whether the coverage is associated with an insurance policy, or a group health plan. For example, enrollees, dependents, participants, beneficiaries are all considered members.
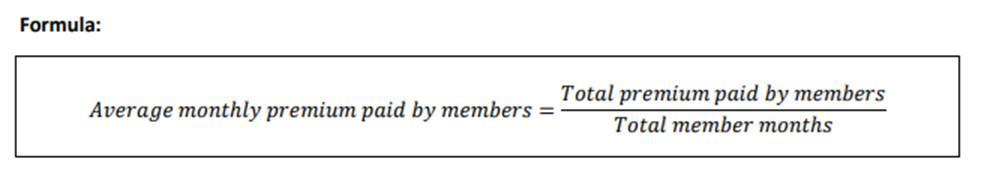
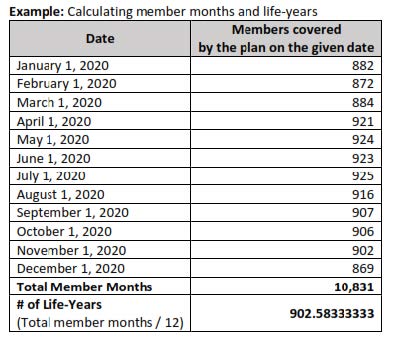
Also from CMS is an example of how to calculate the member months:
- Count the number of members covered on a given day of each month of the reference year
- Add the number of members from Step 1 to calculate total member months for the reference year
- To calculate the life years, divide the member months by 12
- Round the resulting number to the 8th decimal place
- Please do not include the following:
- Any part of the premium paid by the employer or other plan sponsors on behalf of the member
Average Monthly Premium Paid by the Employer
For group health plans employers must report the average monthly premium paid by the employers on behalf of members.
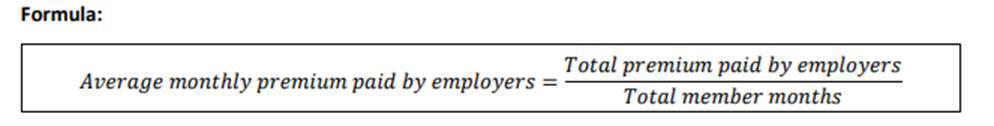
For this calculation employers should include:
- Premiums paid by employers and other plan sponsors on behalf of members (including dependents)
For this calculation they should exclude:
- Any premiums paid by members
Action Items
United Healthcare Deadline: March 3, 2023
- UHC will not be sending new links to clients so clients will have to keep their eyes open for the email coming from UHC
- This includes any clients with a UHC plan at any time during 2022
- Once the survey has been completed you will not be able to go modify or make changes.
- Please use the UHC worksheet to prepare your responses PRIOR to clicking on the survey link
Blue Cross Blue Shield Deadline: March 17, 2023
- Clients can access the survey by clicking HERE
Aetna: March 1, 2023
- Clients can access the survey HERE
Cigna: TBA
Enforcement
If a group does not submit the data requested by the applicable deadlines the carriers will submit to CMS an incomplete record for that group. The group data will not be complete without the required information gathered in the survey and the group will need to submit this data directly to CMS through the HIOS platform no later than June 1, 2023 to avoid any potential penalties.

